Understanding the workers compensation doctor approval process is vital for employees and employers navigating complex systems when workers are injured or develop job-related conditions. Workers comp doctors approve treatments like chronic pain relief and physical therapy, ensuring medical expenses are covered under insurance. Approvals vary based on injury type, doctor availability, and case specifics. Employers initiate the process by reporting incidents and submitting medical info, with insurers consulting approved doctors to determine appropriate treatment according to legal guidelines. The timeline for approvals varies from 1-2 weeks (with accurate docs) to several days/months for complex treatments, emphasizing efficient communication between all parties.
Unsure about the timeline for workers compensation doctor approvals? This comprehensive guide breaks down the intricate process, from initial claim submission to final approval. We explore the key stages involved, offering valuable insights into the factors that can expedite or delay decisions. Understanding these timelines is crucial for both employees and employers navigating the complex landscape of workers’ compensation healthcare approvals. Discover how to optimize the process and ensure efficient access to necessary medical care.
- Understanding the Workers Compensation Doctor Approval Process
- Key Stages in Obtaining Doctor Approvals for Claims
- Timeframes and Factors Affecting Approval Decisions
Understanding the Workers Compensation Doctor Approval Process

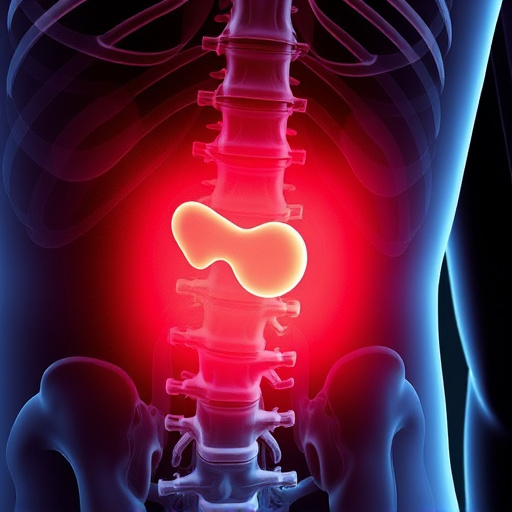
Understanding the Workers Compensation Doctor Approval Process is crucial for both employees and employers navigating this complex system. When a worker sustains an injury or develops a condition related to their job, they often require specialized care. In such cases, workers compensation doctors play a pivotal role in approving necessary treatments, including chronic pain relief and personalized treatment plans that may involve physical therapy. This approval process ensures that the medical expenses are covered under the workers’ compensation insurance, providing financial security for the worker while facilitating access to quality healthcare.
The timeline for these approvals can vary, influenced by factors such as the nature of the injury or illness, the availability of specialized doctors, and the specific requirements of each case. Employers bear responsibility for initiating the process by reporting the work-related incident and submitting relevant medical information. Once received, insurance carriers will assess the claim and consult with approved workers compensation doctors to determine the appropriate course of treatment, ensuring that every step aligns with the worker’s best interests while adhering to legal guidelines.
Key Stages in Obtaining Doctor Approvals for Claims

Obtaining doctor approvals for workers compensation claims involves several key stages that can impact the timeline and outcome of the process. Initially, the injured worker must seek immediate medical attention to diagnose the injury and establish a treatment plan. This often includes referrals to specialists like chiropractors or physiotherapists, focusing on non-invasive treatments to manage pain and promote healing.
Throughout this period, the healthcare provider documents the patient’s condition, treatments, and progress. These records become crucial for submitting claims to the workers compensation insurance carrier. The insurer reviews these submissions, potentially involving consultations with their own medical experts, to approve or deny coverage for recommended treatments, including chiropractic care and pain management strategies. Efficient communication between all parties is vital to navigate this process effectively.
Timeframes and Factors Affecting Approval Decisions

The timeline for workers compensation doctor approvals can vary significantly based on several factors. Key considerations include the complexity of the medical case, the type and extent of injuries, and the availability of relevant medical records. In general, initial requests for approval often take 1-2 weeks to process, provided all necessary documentation is submitted accurately. However, if additional information or clarification is required, this timeframe can extend by several days or even up to a month.
Unique circumstances like specialized treatments, such as mobility improvement techniques or post-injury care plans, can introduce further delays. For conditions requiring sciatica relief or other complex interventions, insurers may seek second opinions or consult with medical experts, which adds an additional layer of review. While these processes are essential for ensuring accurate compensation and proper post-injury care, they contribute to longer approval timelines.
Understanding the timeline for workers’ compensation doctor approvals is crucial for both employers and employees. By grasping the key stages and factors influencing approval decisions, you can navigate the process more effectively. Timely approvals ensure injured workers receive necessary treatments while minimizing claims costs. For medical professionals, adhering to guidelines and providing comprehensive reports can expedite the process, ultimately fostering a smoother experience in the complex world of workers’ compensation medicine.